Table of Contents
I. Understanding Strokes and Blood Thinners
II. Factors Influencing Blood Thinners’ Efficacy
III. How Much Do Blood Thinners Reduce the Risk of Stroke?
How much do blood thinners reduce the risk of stroke? It’s an important question for people taking these medications—especially those with a particularly high risk of stroke occurrence.
We know that blood thinners inhibit the formation of blood clots, maintaining a smooth blood flow and reducing the chances of blockages that lead to stroke. That said, knowing their true efficacy, risk factors, and side effects is crucial for making smart treatment decisions and optimizing health outcomes.
In this article, we’ll explore exactly how much blood thinners reduce the risk of stroke for patients and ways patients and providers can work together to lower stroke risks as much as possible. Whether you’re already taking blood thinners or may in the future, this guide will help you understand your full risk and the best prevention strategies you can take alongside your medication regimen.
Quick Takeaways:
- Blood thinners reduce the risk of stroke by preventing blood clot formation.
- There are two types of blood thinners: anticoagulants and antiplatelets. The best medication and treatment plan depends on each patient’s needs and guidance from a healthcare provider.
- For decades, clinical trials have proven the efficacy of blood thinners in preventing stroke.
- Price can also be a factor in patient adherence and, ultimately, blood thinner efficacy. My Drug Center offers affordable options for ordering blood thinners.
Understanding Strokes and Blood Thinners
A stroke occurs when the blood supply to a part of the brain is interrupted or reduced, depriving brain tissue of oxygen and nutrients. This can lead to brain cells dying within minutes.
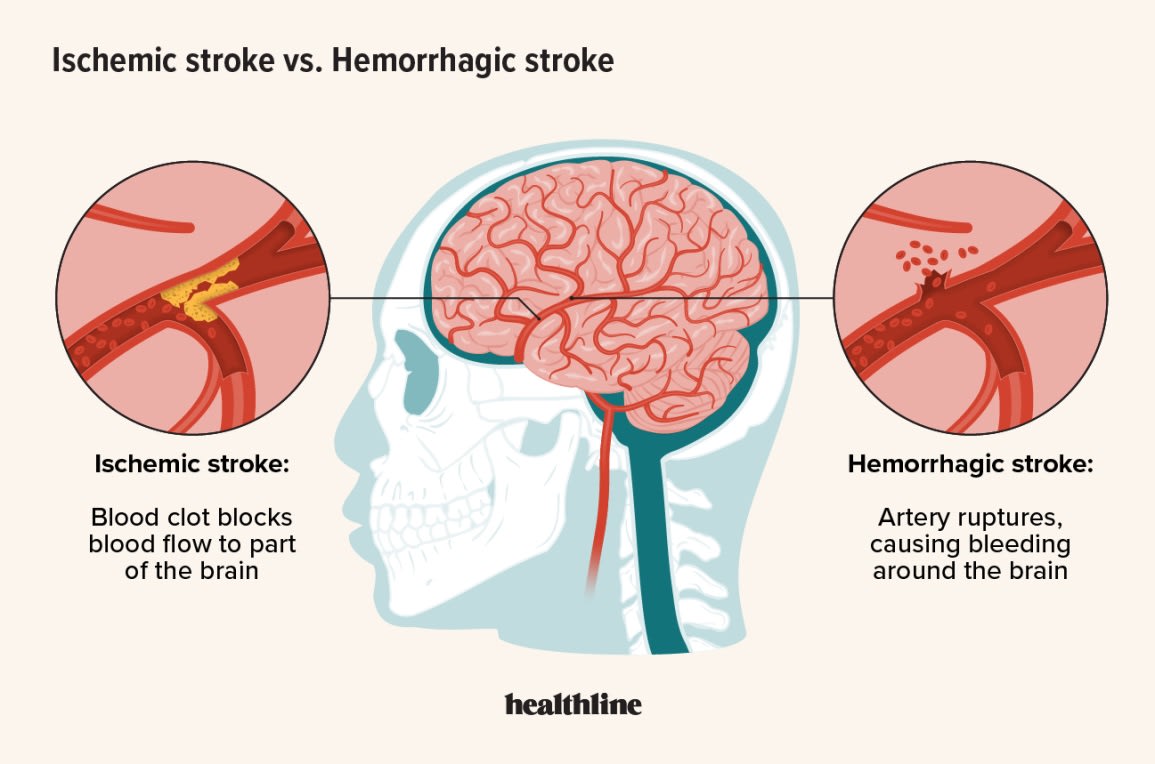
There are two main types of strokes: ischemic and hemorrhagic. Ischemic strokes, the most common type, occur when a blood clot blocks or narrows an artery leading to the brain. Hemorrhagic strokes occur when a blood vessel in the brain bursts, leading to bleeding in or around the brain. Both can have devastating impacts on health, causing physical and cognitive disabilities and significantly affecting quality of life.
Blood thinners are medications designed to prevent strokes by inhibiting the formation of blood clots. They work by interfering with the blood's ability to clot, ensuring that blood flows smoothly through the arteries and veins.
There are two main types of blood thinners: anticoagulants and antiplatelets. Anticoagulants, such as Warfarin and Dabigatran, reduce the formation of blood clots by targeting various factors in the clotting process. Antiplatelets, like Aspirin and Clopidogrel, prevent platelets from clumping to form clots.
Both types of blood thinners play a crucial role in reducing the risk of ischemic strokes by preventing the blockages that can lead to these events, helping to protect brain health and maintain quality of life.
Factors Influencing Blood Thinners’ Efficacy
The effectiveness of blood thinners in preventing strokes varies based on several factors. Patient-specific factors, such as age, medical history, and genetic predispositions, play a significant role. Older patients or those with a history of heart disease may respond differently to blood thinners.
Additionally, genetic variations affect how a patient metabolizes these medications, influencing their efficacy and risk of side effects. Lifestyle choices, including diet, exercise, and adherence to medication regimens, are also crucial. Consistent medication use as prescribed is essential for maintaining the protective effects of blood thinners.
The type of blood thinner prescribed can also impact its effectiveness. As mentioned, different blood have varying mechanisms of action, efficacy rates, and side effect profiles. For instance, Warfarin requires regular blood monitoring and dietary restrictions to maintain its effectiveness, whereas newer anticoagulants like Xarelto and Eliquis typically do not require frequent monitoring and have fewer dietary interactions.
The choice of blood thinner must be tailored to each patient's specific needs and medical condition, considering both the benefits and potential risks. Proper dosage and monitoring are critical to the effectiveness of blood thinners. Adhering to prescribed dosages and following monitoring guidelines helps maximize the benefits of blood thinners while minimizing potential complications, ensuring optimal protection against stroke.
How Much Do Blood Thinners Reduce the Risk of Stroke?
Blood thinners significantly reduce the risk of stroke, particularly ischemic strokes, which are the more common type. Anticoagulants like warfarin have been found to reduce the risk of stroke by approximately 64% in patients with atrial fibrillation. [2] Newer anticoagulants like rivaroxaban (Xarelto) and apixaban (Eliquis) have demonstrated similar or even superior efficacy, along with the added convenience of less frequent monitoring.
Antiplatelet medications such as aspirin and clopidogrel are also effective in reducing the risk of recurrent strokes, especially in patients with a history of stroke or transient ischemic attacks, reducing the risk of serious vascular events, including stroke, by about 20%. [3]
It’s important to reemphasize that consistent adherence to prescribed medication regimens and lifestyle choices like diet and exercise are also crucial for maximizing their efficacy. Regular monitoring and dosage adjustments, particularly for medications like warfarin that require INR testing, help maintain the delicate balance between preventing clots and avoiding excessive bleeding.
Finally, blood thinner effectiveness is maximized when medication choices and regimens are tailored to each individual patient's needs. These medications, when used correctly, can offer substantial protection against strokes, significantly improving long-term health outcomes.
Final Takeaway
There’s no doubt that blood thinners are highly effective in reducing the risk of stroke—particularly ischemic strokes—by inhibiting blood clot formation. That said, many factors play a role that require the careful selection of the right medication, dosage, and monitoring plan. This should be done in close consultation with a professional healthcare provider.
Price can also significantly impact a patient’s ability to access medication and adhere to their treatment plan, which is why My Drug Center offers affordable options that save customers up to 80% on their blood thinner prescriptions.
Learn more about ordering from My Drug Center by visiting our ordering page or contacting our customer service team today.
DISCLAIMER: The information in the article is not meant to be used for treatment or diagnosis. It is designed for general awareness and for information purposes only. Always consult a medical professional for your specific healthcare needs.
