Table of Contents
I. Understanding the Concept of Diabetes Reversal
II. Reversing Diabetes: Lifestyle Changes and Medical Interventions
III. Key Considerations for Long-Term Outcomes
Diabetes is a chronic condition that affects hundreds of millions of people worldwide. It’s characterized by elevated blood sugar levels, leading to serious health issues when not managed properly. Among those diagnosed, a common and pressing question often arises: Can you reverse diabetes? This no doubt reflects the hope and desire for a solution beyond dealing with lifelong management of the condition.
The short answer is yes, it’s possible to reverse diabetes. But the answer is much more complex, and it depends on several factors for any given individual.
In this article, we’ll explore the science behind diabetes reversal and the challenges that individuals may face on this journey. Our aim is to provide a comprehensive overview of current knowledge and practical advice to help you understand the potential for reversing diabetes in your specific situation.
As you read this guide, remember that any attempt to reverse diabetes must be made in close consultation with your healthcare provider.
Quick Takeaways:
- Type 2 diabetes can potentially be reversed through significant lifestyle changes and medical interventions, leading to remission.
- Reversing diabetes focuses on achieving normal blood sugar levels without medication, differentiating remission from a cure.
- Diet and significant weight loss play crucial roles in managing and potentially reversing Type 2 diabetes.
- Bariatric surgery and medication adjustments are effective medical interventions that can support diabetes remission efforts.
- Long-term diabetes remission requires maintaining lifestyle changes, personalized treatment plans, and ongoing monitoring by healthcare professionals.
Understanding the Concept of Diabetes Reversal
Diabetes, a chronic condition marked by elevated blood sugar levels, manifests in two primary forms: Type 1 and Type 2.
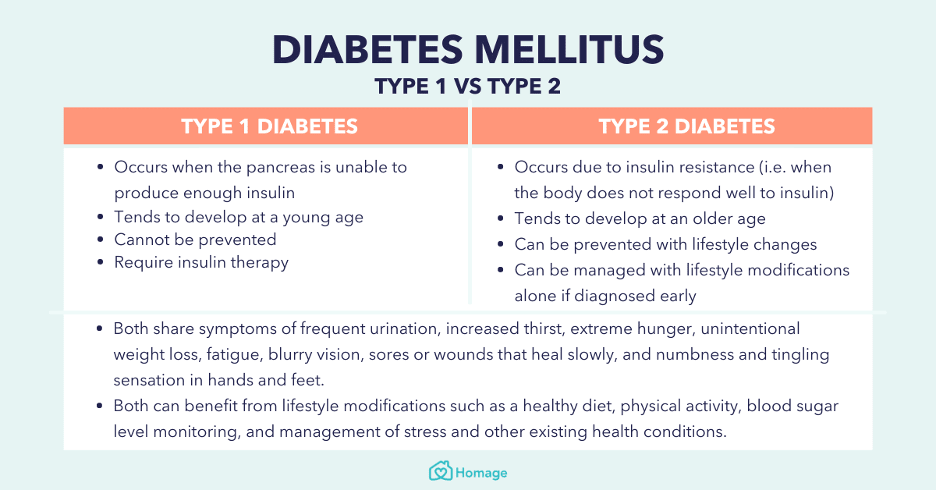
Type 1 diabetes is an autoimmune condition in which the pancreas doesn’t produce enough insulin, necessitating lifelong insulin administration. Type 2 diabetes is more prevalent, arising from the body's inability to use insulin effectively. It’s often linked to lifestyle factors like obesity or physical inactivity.
Both Type 1 and Type 2 diabetes carry significant health risks that include heart disease, kidney failure, vision loss, and neuropathy, making diligent management vital to prevent these serious complications.
The concept of reversing diabetes predominantly refers to Type 2 diabetes and involves significant lifestyle changes that can lead to the reduction of blood sugar levels back to a normal range, potentially allowing individuals to reduce or eliminate the need for medication.
This concept does not imply a permanent cure but rather a state of remission where the disease's effects are minimized. Remission can be partial or complete, depending on whether blood sugar levels are only partially controlled or consistently fall within the non-diabetic range without medication.
The distinction between remission and a cure is crucial. A cure would mean the disease has been entirely eradicated and there's no risk of its return, which is not currently possible for diabetes. Remission, however, indicates that while the underlying risk factors for the disease may still be present, they’re being managed well enough that the disease's symptoms and risks are significantly reduced.
Diabetes remission is widely acknowledged by modern research and leading organizations such as The American Diabetes Association and Diabetes UK, suggesting that for some people with Type 2 diabetes, it's possible to maintain blood sugar levels within a healthy range with the daily use of medication. [2] [3]
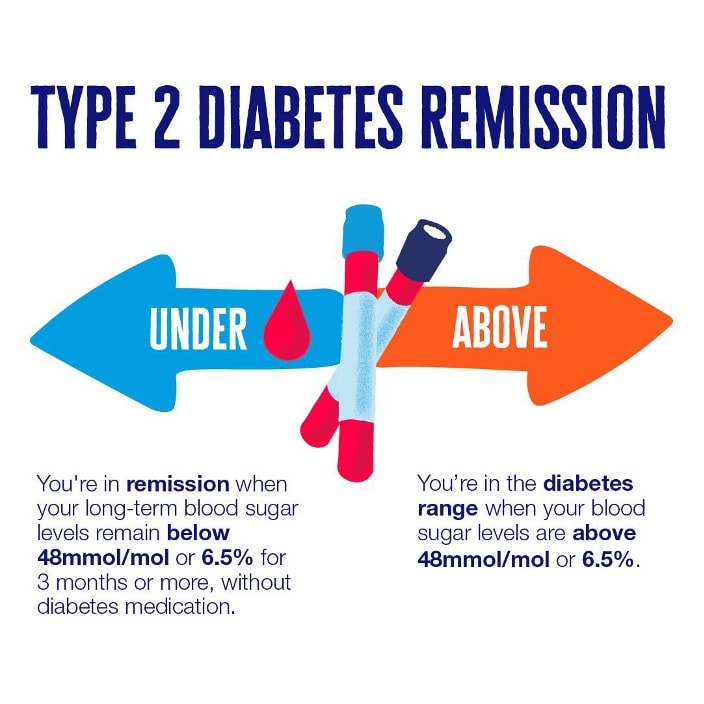
That said, the possibility of diabetes symptoms returning requires permanent lifestyle management and medical supervision, even when symptoms are not present.
Reversing Diabetes: Lifestyle Changes and Medical Interventions
The journey towards reversing Type 2 diabetes (T2D) can encompass both lifestyle modifications and medical interventions, each playing a pivotal role in managing the disease. By addressing the root causes of T2D, such as obesity and insulin resistance, individuals can significantly impact their diabetes status, moving towards remission and potentially reversing the condition.
Lifestyle Changes and Weight Loss
Diet plays a fundamental role in managing and potentially reversing Type 2 diabetes. Adopting a nutritious, balanced diet that focuses on whole foods, minimizes processed sugars, and incorporates plenty of fiber can help stabilize blood sugar levels and improve insulin sensitivity.
Moreover, significant weight loss, often achieved through a combination of diet and increased physical activity, has been shown to have a profound impact on diabetes remission. Studies have demonstrated that individuals who achieve and maintain substantial weight loss can reduce their dependence on diabetes medications, with some even achieving complete remission. [4]
Medical Interventions
Bariatric surgery is also an effective intervention for reversing Type 2 diabetes in obese individuals. Procedures such as gastric bypass and sleeve gastrectomy facilitate significant weight loss and alter hormones and gut bacteria that influence blood sugar control. Many patients experience a dramatic improvement in their diabetes status post-surgery, with a substantial number achieving remission.
Additionally, medication adjustments play a crucial role in managing Type 2 diabetes. Newer classes of diabetes medications can improve blood sugar control and, in some cases, contribute to weight loss, further supporting efforts toward remission. Collaborating closely with a healthcare provider to tailor medication regimens is essential in these cases.
Key Considerations for Long-Term Outcomes
Achieving long-term remission of Type 2 diabetes presents challenges, including the difficulty of maintaining lifestyle changes and weight loss over time. Personalized treatment plans are crucial, as they cater to individual health conditions, preferences, and lifestyle factors.
Healthcare professionals must monitor patients on an ongoing basis to adjust treatment plans as needed and address any emerging health issues promptly. Recognizing challenges and concerns is also important to setting realistic expectations and achieving sustainable outcomes in diabetes management.
If diabetes medication is part of your treatment plan right now, My Drug Center can help. We offer a safe and affordable channel for ordering diabetes medication, and convenient at-home delivery to make the whole process easy. Learn more here about how to save on your next prescription.
The information in the article is not meant to be used for treatment or diagnosis. It is designed for general awareness and for information purposes only. Always consult a medical professional for your specific healthcare needs.
