Table of Contents
I. Initial Stages of Type 2 Diabetes
II. How Does Type 2 Diabetes Progress?
III. Slowing the Progression of Type 2 Diabetes
Type 2 diabetes affects millions of people worldwide. Unlike type 1 diabetes, which is an autoimmune condition, type 2 diabetes is largely influenced by lifestyle factors and genetics.
Understanding how type 2 diabetes progresses over time is crucial for effective management and to prevent complications. As the disease advances, the body's ability to produce and use insulin effectively diminishes, leading to higher blood sugar levels and an increased risk of serious health issues. Early detection and proactive management can significantly slow the progression of the disease and enable people with type 2 diabetes to lead a healthier, fuller life.
This article aims to answer this key question: How does type 2 diabetes progress over time? By exploring the stages of disease progression, the factors that influence it, and the management strategies available, we’ll provide a comprehensive guide for patients and caregivers.
Quick Takeaways:
- Pre-diabetes indicates that a person is at risk of developing type 2 diabetes. It’s characterized by symptoms including frequent urination, fatigue, and blurred vision.
- Type 2 diabetes progresses when β-cell function deteriorates and causes prolonged high blood sugar.
- Individuals with genetic predisposition to type 2 diabetes can have up to a 70% risk of developing the condition.
- Healthy diet, exercise, and adherence to medication plans can slow down diabetes progression.
Initial Stages of Type 2 Diabetes
Pre-diabetes is a condition where blood glucose levels are higher than normal but not yet high enough to be classified as type 2 diabetes. It serves as a warning sign that a person is at higher risk of developing diabetes. Characteristics of pre-diabetes include elevated fasting blood sugar levels and impaired glucose tolerance. Insulin resistance, where the body's cells become less responsive to insulin, is also a sign of pre-diabetes. Common symptoms of pre-diabetes and insulin resistance include:
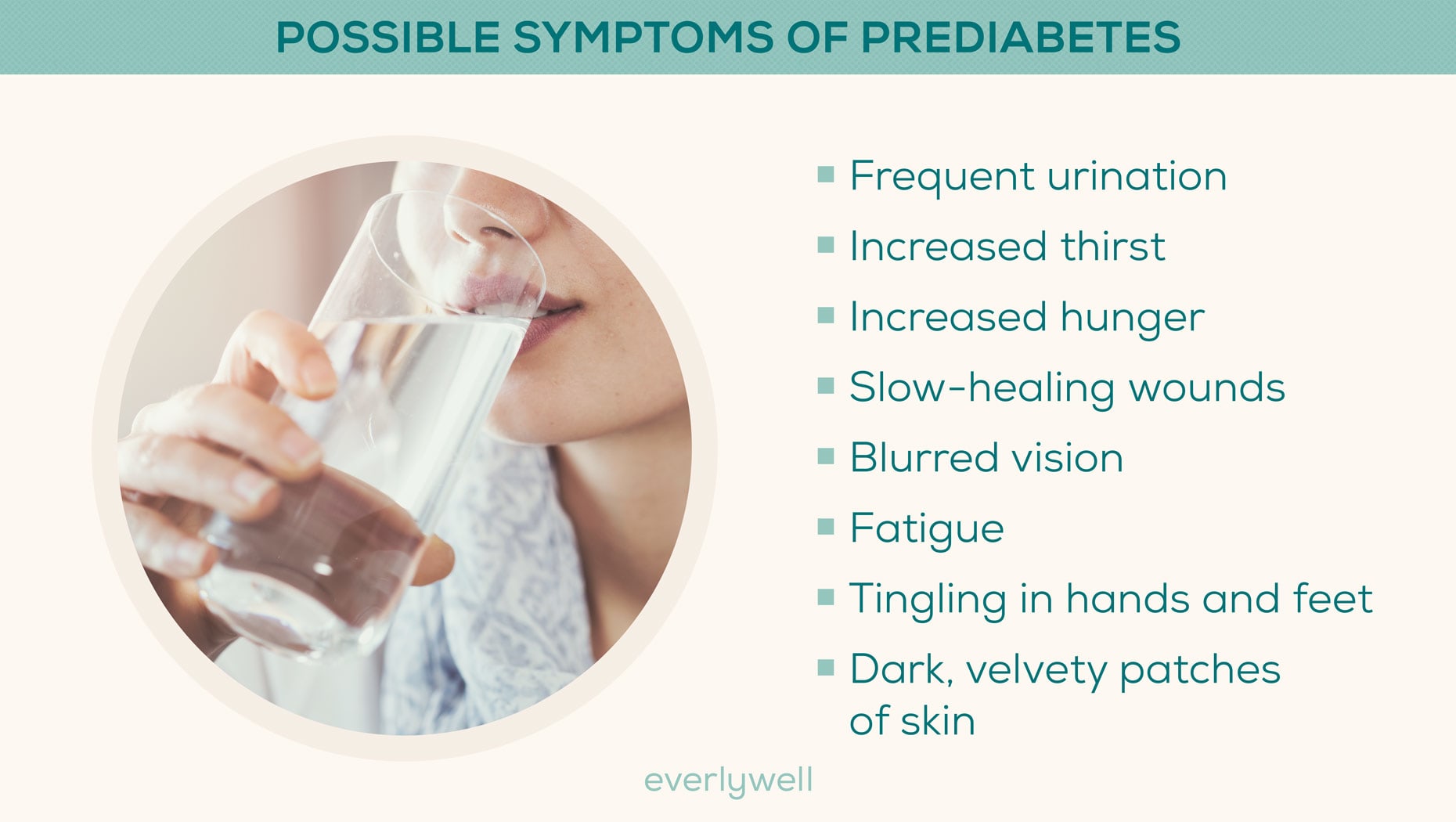
- Increased thirst
- Frequent urination
- Fatigue
- Increased hunger
- Blurred vision
- Unexplained weight change
- Dark patches of skin
- Tingling in hands and feet
Early detection of pre-diabetes is crucial because it offers an opportunity to make lifestyle changes that can slow or even prevent the progression to type 2 diabetes. By adopting healthier eating habits, increasing physical activity, and managing weight, they can improve insulin sensitivity and lower blood glucose levels.
How Does Type 2 Diabetes Progress?
The deterioration of β-cell function in the pancreas is a gradual process that significantly impacts the body's ability to produce insulin. Over time, β-cells become less efficient and eventually fail to meet the body's insulin demands.
This decline in function is a result of prolonged high blood sugar levels, which cause stress and damage to the β-cells. As β-cell function deteriorates, the body's capacity to regulate blood glucose diminishes, leading to increasingly elevated blood sugar levels and, eventually, the progression of type 2 diabetes.
Initially, this may be managed by increased insulin production, but as β-cell function declines further, this compensatory mechanism fails. Factors influencing the increase in blood glucose levels include genetic predisposition, diet, physical activity, and overall health. Poor dietary choices, lack of exercise, and obesity can accelerate the rise in blood glucose levels.
As type 2 diabetes progresses, it can lead to various complications. Cardiovascular issues are common, with an increased risk of heart disease and stroke. Neuropathy, or nerve damage, can result in pain, tingling, and loss of sensation, particularly in the extremities. Retinopathy, which affects the eyes, can cause vision problems and potentially lead to blindness if not managed properly.
The long-term health implications of unmanaged type 2 diabetes are severe and can significantly impact quality of life. Chronic high blood sugar levels can lead to kidney disease, which may progress to kidney failure. Additionally, the risk of infections and slow wound healing can result in serious complications and even amputations.
All this said, type 2 diabetes can be managed effectively so that individuals with the condition can lead a healthy life. Lifestyle changes, medication adherence, and frequent monitoring are crucial to mitigating long-term health risks and improving overall health outcomes.
Slowing the Progression of Type 2 Diabetes
Despite its many potential complications, type 2 diabetes can be managed effectively to slow its progression and allow individuals with the condition to live a full and healthy life. These are some of the most important strategies for controlling diabetes and minimizing its impact:
1. Understanding Factors Influencing Disease Progression
Genetics play a significant role in the progression of type 2 diabetes. Individuals with a family history of diabetes are at a higher risk of developing the condition themselves. In fact, people with one parent who has type 2 diabetes have a 40% risk of developing it themselves, and that risk jumps to 70% when both parents have the condition. [2]
Genetic predisposition can affect how the body produces and uses insulin, influencing the rate of diabetes progression. Getting informed about your family history is important to understanding your personal diabetes risk.
2. Make Lifestyle Adjustments
Adopting a healthy diet rich in whole grains, vegetables, lean proteins, and healthy fats can help manage blood glucose levels. Below, you can learn more about what a person with type 2 diabetes should eat:

Regular exercise, such as walking, swimming, or cycling, improves insulin sensitivity and helps maintain a healthy weight. Incorporating foods with a low glycemic index and engaging in both aerobic and resistance training exercises can be particularly beneficial.
3. Adhere to Medical Interventions
Medications are available to help manage blood glucose levels. It’s essential to consult with your doctor about potential medication interventions and follow the prescribed treatment plan. Regular blood glucose monitoring and routine check-ups with healthcare professionals are vital to adjusting treatment plans as needed and addressing any complications early.
4. Advanced Treatment Options
For some individuals, insulin therapy may become necessary as the disease progresses. Other advanced treatments, including GLP-1 receptor agonists like Rybelsus or Ozempic, can also help manage the condition. Technologies like continuous glucose monitors provide real-time blood sugar readings and enable better management of type 2 diabetes.
Taking Action
By understanding and addressing factors that impact type 2 diabetes progression and implementing effective management strategies, individuals can slow the disease's progression and improve their overall health and well-being.
At My Drug Center, we are committed to helping you manage your type 2 diabetes effectively. Our pharmacy offers a wide range of diabetes medications at affordable prices, ensuring you have access to the treatments you need.
Visit our homepage to learn more about how you can save up to 80% on your next prescription.
DISCLAIMER: The information in the article is not meant to be used for treatment or diagnosis. It is designed for general awareness and for information purposes only. Always consult a medical professional for your specific healthcare needs.
